|
 |
Back to Annual Meeting Program
Predictive Factors of Pancreatic Fistula and Postoperative Complications After Pancreatic Resections in Two High Volume Centers: Comparison Between Posterior Invagination and Duct-to-Mucosa Pancreaticogastrostomy
Filippo Scopelliti*1, Giovanni Butturini1, Carlo Frola2, Mohammad Abu Hilal2, Claudio Bassi1
1Department of Surgery, Verona University, Verona, Italy; 2Hepato Pancreatico Biliary Surgery Unit, Southampton General Hospital, Southampton, United Kingdom
Introduction. Pancreatic fistula (PF) is a major complication after pancreatic resections. Well known risk factors are soft pancreatic remnant and small duct. The most widely used techniques to reconstruct the pancreo-digestive continuity are pancreojejunostomy (PJ) and pancreogastrostomy (PG), either executable by invagination or duct-to-mucosa. Unlike PJ, there are no studies evaluating short term outcome and PF rate comparing invagination versus duct-to-mucosa PG.
Methods. In this dual-institution retrospective study, 345 patients, reconstructed by invagination or duct-to-mucosa PG after pancreatic resections, were stratified in two groups by the type of PG performed. The invagination group consists of 173 patients from 2000 and 2010 at the same institution, selected for having soft pancreatic remnant. The duct-to-mucosa group consists of 172 consecutive patients from 2007 and 2010 at the other institution. Primary end point was to compare the two groups in terms of postoperative complications, including PF rate and grading, as defined by the International Study Group of Pancreatic Fistula. Secondary end point was the assessment of possible predictive risk factors of PF, unrelated to the type of anastomosis.
Results. No differences in demographic data between the two groups were found except of the median age, significantly higher in duct-to-mucosa group (67 vs 62 years; P=0,001). In invagination group 90,1% of patients had a soft pancreatic remnant vs 48,2% in the duct-to-mucosa group (P=0,0001). There were 47 PFs (27,2%) in the invagination group and 44 (25,6%) in the duct-to-mucosa group (P=NS). Furthermore no differences in PF grading were found. The patient in duct-to-mucosa group experienced abdominal collections in 42 cases (24,2%) respect of the 18 patients (10,4%) in the invagination group (P=0,001). Also delayed gastric emptying rate was significantly higher in duct-to-mucosa group, 44 cases (25,6%) respect of the 10 (5,8%) in the invagination group (P=0,0001). Mortality was 0% in invagination group and 4,1% (7 cases) in duct-to-mucosa group, but this difference may be due to the higher median age of this population respect of the invagination group. In multivariate analysis for PF, independent risk factors, unrelated to the type of anastomosis, included sex male (P=0,0001), soft pancreatic remnant (P=0,0001) and small pancreatic duct (P=0,005).
Conclusions. The type of pancreogastrostomy does not significantly influence the overall postoperative complication rate or incidence of PF. However, abdominal collections and delayed gastric emptying are significantly reduced in patients treated by invagination PG. Furthermore invagination seems to be safer than duct-to-mucosa in case of soft pancreatic remnant. In addition, soft pancreatic remnant and small duct can be confirmed as independent risk factors for PF.
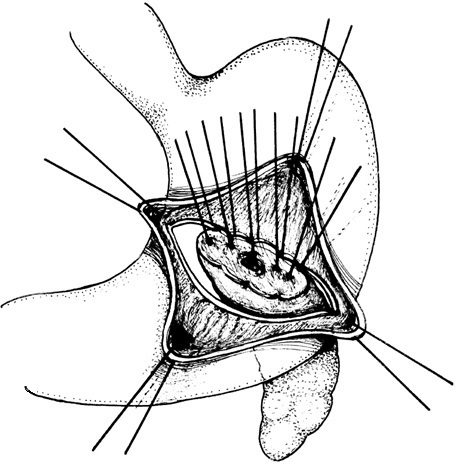
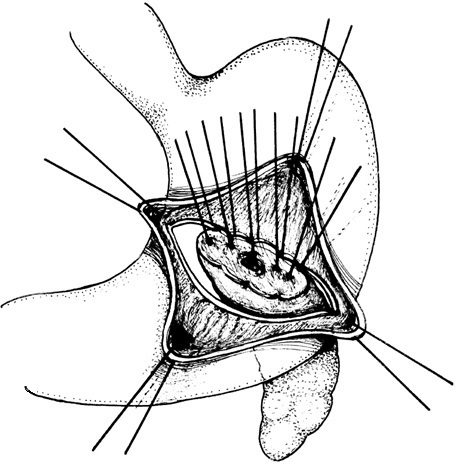
Invagination PG
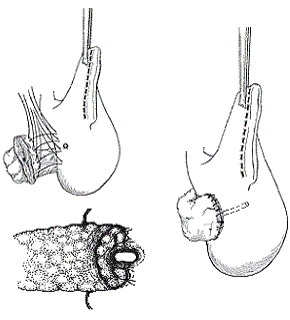
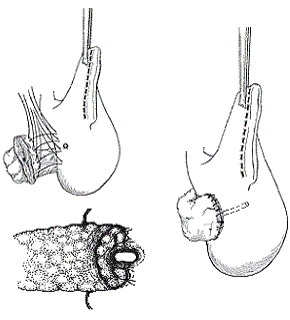
Duct-to-mucosa PG
Back to Annual Meeting Program
|