|
 |
Back to Annual Meeting Program
Contemporary Treatment and Outcomes of Periampullary Adenocarcinomas At a Single Institution
Vei Shaun Siow*, Zhi Ven Fong, Harish Lavu, Eugene P. Kennedy, Patricia K. Sauter, Leonidas Koniaris, Ernest L. Rosato, Charles J. Yeo, Jordan M. Winter
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Periampullary adenocarcinoma (PA) is the most common indication for pancreaticoduodenectomy (PD). The four cancers that comprise the PAs include pancreatic ductal (PDA), ampullary (AA), distal common bile duct (CBDA), and duodenal adenocarcinoma (DA). While PDA has been studied extensively, it is unclear whether these data are applicable to the rarer PAs.
Methods: We queried our institutional PD database for patients treated for PA from November 2005 to October 2011. Out of 650 resections, 390 (60%) patients had PA. Clinicopathologic data were analyzed, and statistical comparisons between PA subtypes were made with respect to PDA, unless otherwise indicated. We aimed to identify the differences in the biology, natural history, and treatment patterns between PAs.
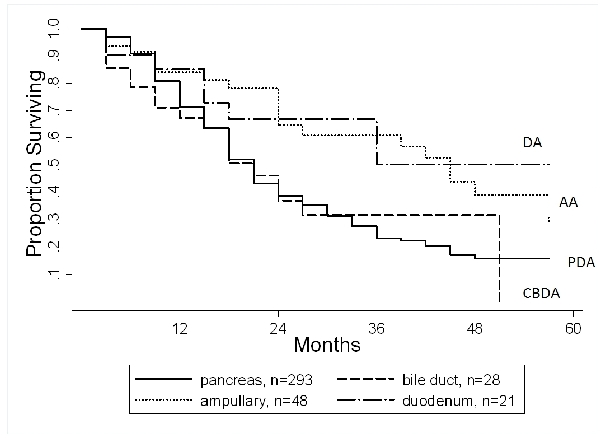
Results: The 390 resected PAs included 293 (75%) PDAs, 48 (12%) AAs, 28 (7%) distal CBDAs, and 21 (5%) DAs. Pre-operative CA 19-9 levels were elevated in 76% of patients with PDA, 56% with distal CBDs (p=0.04), 62% with AA (p=0.071), and 55% with DA (p=0.06). In general, resected PDAs and CBDAs had the more aggressive pathologic features. Specifically, perineural invasion was identified in 92% of PDAs, 93% of distal CBDAs (p=1.0), 51% of AAs (p<0.0001) and 34% of DAs (p<0.0001). Lymph node metastases were identified in 74% of PDAs, 50% of distal CBDAs (p=0.013) 60% of AAs (p=0.05) and 57% of DAs (p=0.1). Documented recurrence patterns were available in a subset of patients (22%) followed at our own institution. Due to the small number of patients, non-pancreatic PAs were analyzed together. The site of first recurrence was the surgical bed in 24% of PDAs and 20% of non-pancreatic PAs. A distant metastasis was identified in 76% of PDAs and 80% of non-pancreatic PAs (p=1.0). With regards to treatment patterns at our institution (N=158 with treatment data), patients with PDA and distal CBDAs are virtually always treated with adjuvant gemcitabine (91%), as compared to the other two subtypes (55%, p<0.0001) which are frequently treated with a 5-FU based regimen. The median and 2-year survivals associated with each PA were (Figure): PDA, 19 months and 39%; CBDA, 18 months and 37% (p=0.8); AA, 43 months and 65% (p=0.002); and DA, median not reached and 67% (p=0.04). After adjusting for lymph node metastases, AA was still more favorable than PDA (hazard ratio=0.73, p=0.01) while DA showed a trend but was not significantly more favorable (hazard ratio, 0.8, p=0.1).
Conclusions: These findings support the notion that PAs are a heterogeneous group. As compared to AAs and DAs, PDAs had more aggressive pathologic features and worse long-term survival. In addition, CA19-9 was a more sensitive test for PDAs than the non-pancreatic PAs. Our practice patterns approach pancreatobiliary cancers primarily with gemcitabine-based treatment, which differs from the approach with the other subtypes.
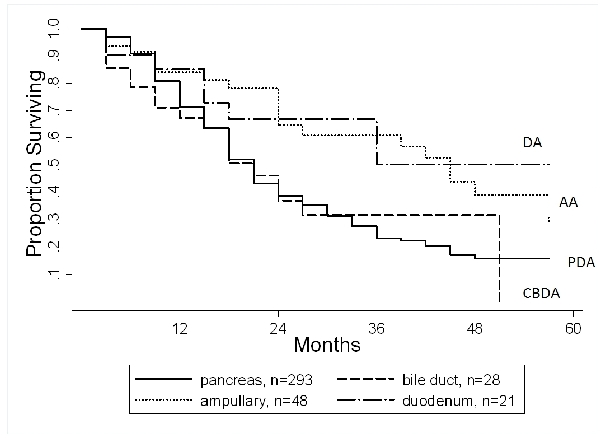
Kaplan-Meier survival curves for patients with periampullary adenocarcinoma.
Back to Annual Meeting Program
|