|
Back to Annual Meeting Program
Quality of Life in Patients After Total Pancreatectomy Is Comparable to Quality of Life in Patients After a Partial Pancreatic Resection
Irene Epelboym*, Megan Winner, Joseph Dinorcia, Minna K. Lee, James a. Lee, Beth Schrope, John a. Chabot, John D. Allendorf
Surgery, New York Presbyterian, Columbia University, New York, NY
Background:
Quality of life after total pancreatectomy is perceived to be poor secondary to insulin-dependent diabetes and pancreatic insufficiency. As a result, surgeons may be reluctant to offer this treatment for benign and premalignant diseases.
Methods:
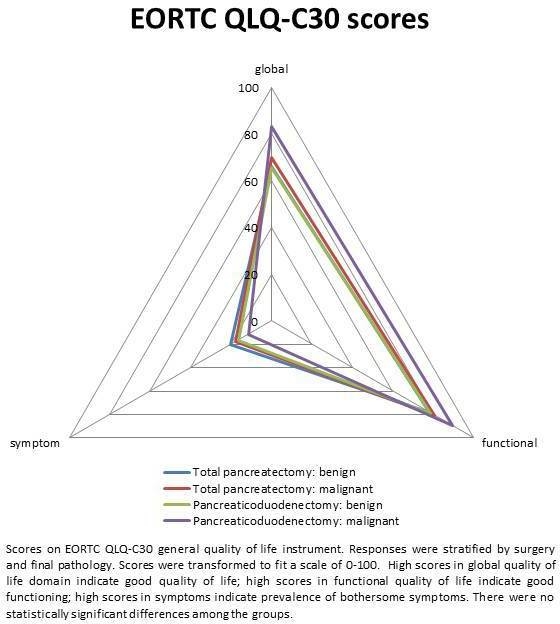
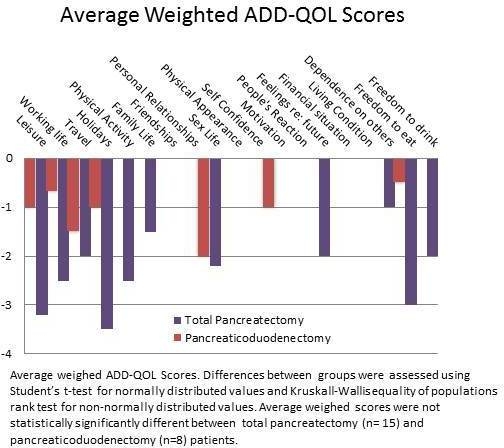
We retrospectively reviewed a prospectively maintained database of pancreatic operations and identified patients who underwent a total pancreatectomy between 1994 and 2011 at our institution. Presenting features, operative characteristics, and postoperative outcomes were evaluated. Quality of life was assessed using institutional questionnaires and validated general, pancreatic disease-related, and diabetes-related instruments (EORTC QLQ-C30, EORTC-PAN26, ADD-QOL) in patients alive at the time of analysis, and compared with frequency-matched controls, patients after a pancreaticoduodenectomy. Continuous variables were compared using Student’s t-test or ANOVA. Categorical variables were compared using chi-square or Fisher’s exact test.
Results:
Between 1994 and 2011, 77 total pancreatectomies were performed, 39 for benign or premalignant, and 38 for malignant disease. Overall morbidity after total pancreatectomy was 49%, but only 12 (16%) patients experienced a major complication. Perioperative mortality was 2.6%. At the time of this study, 33 (43%) patients were alive and 25 agreed to participate in the survey; final results represent aggregate responses of 15 (10 benign and premalignant, 5 malignant). Mean time between surgery and survey administration was 3.2 years. Scores were compared with 14 matched patients who underwent pancreaticoduodenectomy (10 benign and premalignant, 4 malignant; 8 with postoperative diabetes). There were no statistically significant differences in quality of life in the global health, functional status, or symptom domains of the EORTC QLQ-C30 or in the pancreatic disease-specific EORTC-PAN26 between total and partial pancreatectomy patients, regardless of final pathology. Total pancreatectomy patients had slightly but not significantly higher incidence of hypoglycemic events as compared to partial pancreatectomy patients with postoperative diabetes. The negative impact of diabetes as assessed by the ADD-QOL did not differ between total and partial pancreatectomy patients. Life domains most negatively impacted by diabetes involved travel and physical activity, while self-confidence, friendships and personal relationships, motivation, and feelings about the future remained unaffected.
Conclusions:
While total pancreatectomy-induced diabetes negatively impacts select activities and functions, overall quality of life is comparable to that of patients after a partial pancreatic resection.
Back to Annual Meeting Program
|