|
Back to Annual Meeting Program
Extended Left Hepatic Trisectionectomy As a Feasible Surgical Procedure for Advanced Perihilar Cholangiocarcinoma
Minoru Esaki*1, Kazuaki Shimada1, Seiji Oguro1, Yoji Kishi1, Satoshi Nara1, Tomoo Kosuge1, Yoshihiro Sakamoto2, Tsuyoshi Sano3
1Hepato-biliary pancreatic surgery, National Cancer Center Hospital, Tokyo, Japan; 2Hepato-Biliary-Pancreatic Surgery Division, Graduate School of Medicine, University of Tokyo, Tokyo, Japan; 3Department of Gastroenterological Surgery,, Aichi Cancer Center, Nagoya, Japan
Abstract
Objectives: The aim of this study was to clarify the short and long term outcome of extended left hepatic trisectionectomy (LT) for perihilar cholangiocarcinoma.
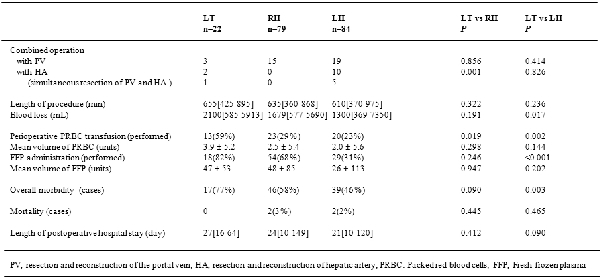
Methods: Patients with perihilar cholangiocarcinoma who underwent LT between January 2000 and October 2010 for perihilar cholangiocarcinoma were analyzed retrospectively. Operative variables, mortality, morbidity, recurrence sites and survival of three groups were compared among LT, right hemihepatectomy (RH) and left hemihepatectomy (LH).
Results: A total 203 patients underwent surgical resection for perihilar cholangiocarcinoma, 22 (11%) of whom underwent LT, 79 (39%) underwent RH, and 84 (41%) underwent LH. No mortality occurred, but 17 patients had morbidity. Operative time and blood loss were 655 ± 142 minutes and 2100 ± 1080 ml, respectively.
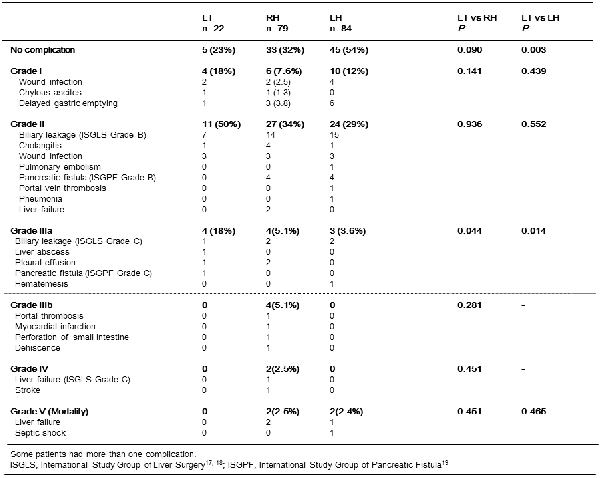
Blood loss in patients with LT was significantly more than in those with LH (2100ml versus 1300ml; P = 0.017). The incidence of Grade IIIa complication in patients with LT was significant higher than RH and LH (P=0.044 and P=0.014), but Grade IIIb and IV complication did not occur in patients with LT. Overall 5-year survival rate was 40% with median survival of 45.8 years. There was no significant difference in survival in patients between LT and other two procedures.
Conclusions: LT for perihilar cholangiocarcinoma is feasible and can provide a comparable prognosis for advanced perihilar cholangiocarcinoma originating from left hepatic duct or segment 4 especially extending to the root of the right anterior portal pedicle or confluence of the anterior and posterior branch of the bile duct.
Back to Annual Meeting Program
|