|
 |
Back to Annual Meeting Program
Quality Assessment in Pancreatic Surgery: What Might Tomorrow Require?
Brian T. Kalish*1, Charles M. Vollmer2, Tara S. Kent1, William H. Nealon3, Jennifer F. Tseng1, Mark P. Callery1
1Surgery, Beth Israel Deaconess Med Ctr, Boston, MA; 2Surgery, University of Pennsylvania, Philadelphia, PA; 3Surgery, Vanderbilt University, Nashville, TN
INTRODUCTION: The Institute of Medicine (IOM) defines healthcare quality across six domains: safety, timeliness, effectiveness, patient centeredness, efficiency, and equitability. Traditional quality metrics in high-acuity surgery (volume and mortality) cannot alone measure or satisfy these domains. We asked experts in pancreatic surgery (PS) whether broader quality metrics are needed, how important they might be, and whether they align to contemporary IOM healthcare quality domains.
METHODS: Together with a professional market research firm, we created and distributed a web-based survey to pancreatic surgeons. These experts were identified through PS specialty societies, and verified by survey demographics. Respondents (Rpds) ranked 62 proposed PS quality metrics on level of importance (LoI). Next, Rpds aligned each metric to one or more IOM quality domains (MDA, multi-domain alignment). Descriptive statistics were used to summarize responses. To calculate and rank relative quality scores, points were awarded for LoI (4-Essential, 3-Very important, 2-Somewhat important, 1-A Little important, 0-Not important) and MDA (1 point/each aligned domain). LoI Scores and MDA Scores for a given quality metric were averaged together to render a Total Quality Score (TQS=LoI + MDA/2) normalized to a 100-point scale.
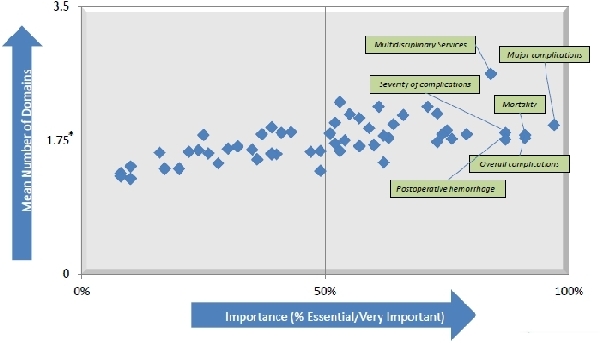
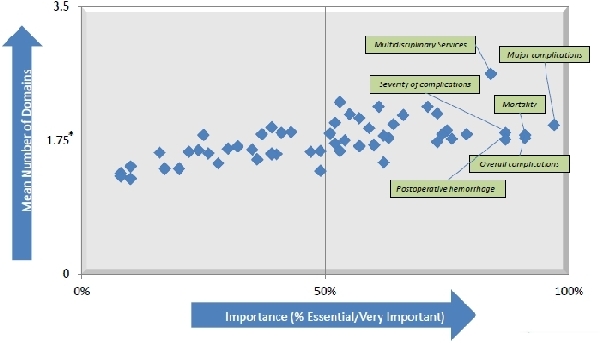
RESULTS: 106 surgeons (21%) completed the survey (82% North America and 84% Academic). On average, Rpds and their institutions perform 43 and 114 pancreatic operations per year, respectively. By descriptive analysis, 90% of Rpds indicated a definite or probable need for improved quality metrics in PS. 81% of Rpds indicated a definite or probable value for a “Quality Scorecard” in PS. Of 13 PS quality metrics rated as Essential by >25% Rpds, 10 aligned most strongly to the IOM Safety domain. 22/62 proposed metrics aligned to more than 1.75 IOM Domains, and were rated by >50% Rpds as High LoI (Essential or Very Important; Figure). 12 proposed scorecard metrics (Table) emerged with the highest TQS. Those related to mortality, to the rate and severity of complications, and to access to multidisciplinary services for pancreatic disease had the highest TQS. Technical and peri-operative metrics had intermediate TQS. Metrics related to patient satisfaction with care, costs of care, and patient demographics had the lowest TQS. The least represented IOM domains were equitability, efficiency, and patient-centeredness.
CONCLUSIONS: We propose a 12-item "Quality Scorecard" for PS based on rank-scoring of quality metrics that PS experts view as both highly important and aligned with more than one IOM healthcare quality domain. While the actual performance thresholds for these metrics require further definition and validation, they may reveal quality to an extent that volume and mortality alone cannot.
Top Pancreatic Surgery “Quality Scorecard” Metrics by Total Quality Score (TQS)
| Metric | TQS | | Multidisciplinary services for pancreatic diseases | 63 | | Major complication rate | 60 | | Peri-operative mortality (0-90 days) | 59 | | Overall complication rate | 57 | | Incidence of post-operative hemorrhage | 55 | | Venous thromboembolism (VTE) prophylaxis | 54 | | Patients with malignancy who undergo adjuvant therapy | 54 | | Readmission rates (30 day, 90 day, total) | 54 | | Incidence of post-operative pancreatic fistula | 54 | | Timely and appropriate peri-operative antibiotics | 53 | | Survival rates (1 yr and 5 yr post-operative) | 52 | | Timing from diagnosis to surgical consultation | 51 |
Back to Annual Meeting Program
|