|
Back to Annual Meeting Program
Greater Complexity of Liver Surgery Is Not Associated With an Increased Incidence of Liver Related Complications Except for Bile Leak: an Experience With 2628 Consecutive Resections
Robert E. Roses*, Giuseppe Zimmitti, Thomas Aloia, Andreas Andreou, Steven Curley, Jean-Nicolas Vauthey
Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX
Background: Advances in technique, technology and perioperative care have allowed for the more frequent performance of complex and extended hepatic resections. The purpose of this study was to determine if this increasing complexity has been accompanied by a rise in liver related complications.
Methods: A large prospectively maintained single institution database of patients who underwent hepatic resection was utilized to identify the incidence of liver related complications. Patients were divided into two groups of equal size: an earlier group and a later group (surgery performed before or after 5/18/2006). Patient characteristics and perioperative factors were compared between the two groups. Abdominal collection was defined as a non-bilious fluid collection requiring drainage. Bile leak was defined as bilious drainage from the postoperative drain or incision for 3 days or more, or a bilious collection requiring drainage or reoperation. Hemorrhage was defined as bleeding requiring reoperation. Hepatic insufficiency was defined as a peak serum bilirubin level of >7mg/dL at any time postoperatively.
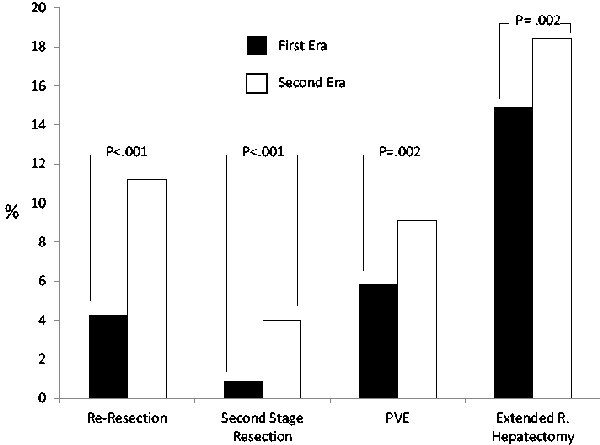
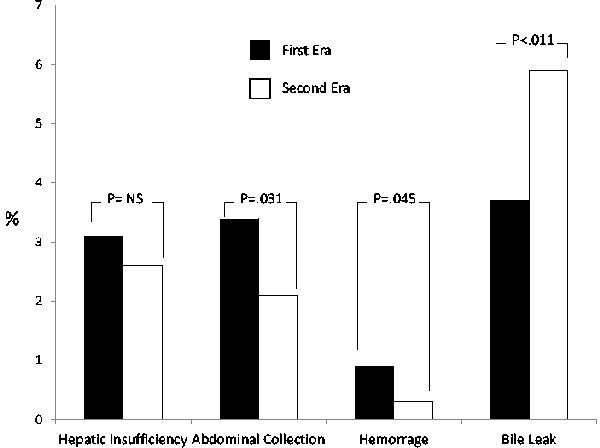
Results: 2628 hepatic resections were performed between 1997 and 2011 with a 90 day morbidity of 37% and mortality of 2%. Comparison of case type between the later and earlier cohorts revealed an increase in complexity over time as evidenced by the greater number of re-resections (11.2% vs 4.3%; p<0.001), second stage resection(4.0% vs 0.9%; p<0.001) and extended right hepatectomies (18.4% vs 14.9%; p=.017) and increasing use of preoperative portal vein embolization (9.1% vs 5.9%; p=0.002) in the later group. Despite this, the incidence of abdominal collection (2.1% vs 3.4%; p=.031) and hemorrhage (0.3% vs 0.9%; p=.045) decreased and the incidence of hepatic insufficiency (2.6% vs 3.1%; p=0.41) remained stable. In contrast, the rate of bile leak increased (5.9% vs 3.7%; p=0.011). For the entire cohort, bile leak was associated with increased 90 day mortality (11.1% vs 1.8%; p<0.001) and increased length of stay (mean 13 vs 8 days; p<0.001). Independent predictors of bile leak included bile duct resection (OR 3.9; p<0.001), resection of >3 segments (OR 3.1; p<0.001), second stage resection (OR 2.5; p=0.019) and intraoperative blood loss> 1 liter (OR 1.9; p=0.019).
Conclusions: Despite an increasing complexity of liver surgery, the rates of liver related complications have remained stable or decreased. An important exception to this is bile leak which has increased in incidence and is now a major cause of surgical morbidity. Given the strong association between bile leak and other poor outcomes, the development of novel technical strategies to reduce bile leak is indicated.
Complexity of Liver Surgery
Liver Related Complications
Back to Annual Meeting Program
|