|
 |
Back to Annual Meeting Program
Neoadjuvant Therapy and Vascular Resection During Pancreaticoduodenectomy: Shifting the Survival Curve for Patients With Locally Advanced Pancreatic Cancer
Joseph Dinorcia*, Megan Winner, Minna K. Lee, Irene Epelboym, James a. Lee, Beth Schrope, John a. Chabot, John D. Allendorf
Surgery, Columbia University College of Physicians and Surgeons, New York, NY
Background: Neoadjuvant chemoradiation therapy and more aggressive surgery with vascular resection are two strategies to bring patients with locally advanced pancreatic cancer to the operating room for potential cure.
Methods: We reviewed the medical records of all patients with pancreatic ductal adenocarcinoma who underwent pancreaticoduodenectomy (PD) at our institution between March 1992 and March 2011. We identified patients who received neoadjuvant (NA) therapy or required major vascular resection and evaluated demographics, operative characteristics, morbidity, mortality, and survival. Student’s t- or Mann-Whitney U tests and Chi-squared or Fisher’s exact tests were used to compare continuous and categorical variables, respectively. Kaplan-Meier curves and Cox proportional hazards models were used to compare survival.
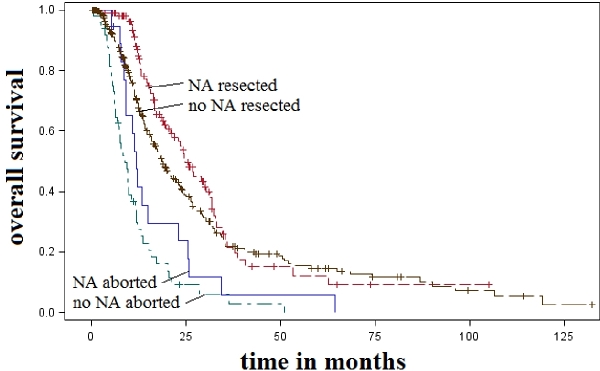
Results: A total of 600 patients were brought to the operating room for attempted resection. One hundred fifty-four (25.6%) had received NA therapy for initially unresectable disease whereas 446 (74.4%) were explored at presentation. One hundred twenty-four (80.5%) NA patients underwent successful PD compared to 340 (76.5%) non-NA patients. The NA patients were younger (62.7 years vs. 67.5 years, p<0.001), more often had prior resection attempts (26.6% vs. 0.9%, p<0.001), had longer median operative times (390 min vs. 328 min, p<0.001), and had higher median estimated blood loss (1500mL vs. 1000mL, p<0.001) than non-NA patients. There were no statistically significant differences in R0 resection rate (82.3% vs. 78.2%, p=0.34), median length of stay (9 days vs. 10 days, p=0.16), morbidity (50% vs. 49.4%, p=0.91), or mortality (6.5% vs. 2.7%, p=0.09) between the two groups. Sixty-one percent of NA patients versus 18.8% non-NA patients required vascular resection (p<0.001), therefore a subset analysis was performed. PD with vascular resection resulted in increased morbidity (54.9% vs. 33.7%, p<0.001) and mortality (1.8% vs. 6.3%, p=0.008), but similar R0 resection rates (74% vs. 81%, p=0.07) and lengths of stay (10 days vs. 9 days, p=0.07) compared to standard PD. Median survival of resected NA patients was similar to resected non-NA patients (24.9 months vs. 19.3 months, p>0.05) and significantly longer than non-NA patients aborted for locally advanced disease (24.9 months vs. 8.9 months, p<0.05). NA patients who required vascular resection had longer survival than non-NA patients who required vascular resection (23.6 months vs. 14.4 months, p<0.05).
Conclusion: Many patients with locally advanced pancreatic cancer can be brought to resection through NA therapy and vascular resection with acceptable morbidity and mortality. These patients have significantly improved survival over patients deemed locally inoperable by traditional criteria.
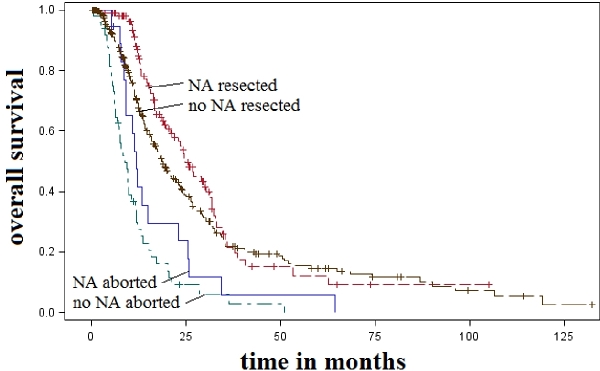
Neoadjuvant (NA) therapy and vascular resection can bring select patients with initially locally unresectable pancreatic cancer to pancreaticoduodenectomy with a significant survival benefit. In this series, median survival of resected NA patients was similar to resected non-NA patients (24.9 months vs. 19.3 months, p>0.05) and longer than non-NA patients aborted for locally advanced disease (24.9 months vs. 8.9 months, p<0.05). Median survival of NA patients aborted for locally advanced disease was 13.3 months.
Back to Annual Meeting Program
|