|
 |
Back to Annual Meeting Program
Improved Long-Term Survival After Major Resection for Hepatocellular Carcinoma: a Multicenter Analysis Based on a New Definition of Major Hepatectomy
Andreas Andreou*1, Jean-Nicolas Vauthey1, Daniel Cherqui2, Eddie Abdalla1, Steven Wei1, Steven Curley1, Alexis Laurent2, Ronnie Poon3, Jacques Belghiti4, David M. Nagorney5, Thomas Aloia1
1Surgical Oncology, M D Anderson Cancer Center, Houston, TX; 2Department of Digestive and Hepatobiliary Surgery and Liver Transplantation, Hôpital Henri Mondor, Créteil, France; 3Department of Surgery, University of Hong Kong/Queen Mary Hospital, Hong Kong, China; 4Department of Surgery, Hôpital Beaujon, Clichy, France; 5Department of Gastroenterologic and General Surgery, Mayo Clinic, Rochester, MN
Background: Advances in the surgical management of hepatocellular carcinoma (HCC) have expanded the indications for curative hepatectomy, including more extensive liver resections. The purpose of this study was to examine long-term survival trends for patients treated with major hepatectomy for HCC.
Patients and Methods: Clinicopathologic data for 1115 patients with HCC who underwent hepatectomy between 1981 and 2008 at 5 hepatobiliary centers in France, China, and the USA were assessed. In addition to other performance metrics, outcomes were evaluated using resection of ≥4 liver segments as a novel definition of major hepatectomy.
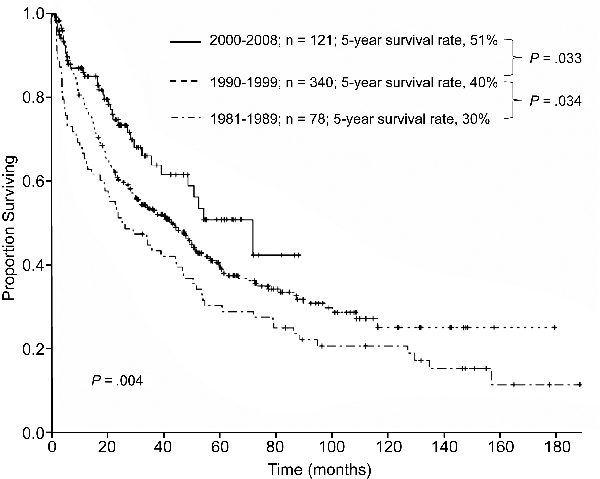
Results: Major hepatectomy was performed in 539 patients. In the major hepatectomy group, median tumor size was 10 cm (range:1-27 cm) and 22% of the patients had bilateral lesions. The TNM Stage distribution included 29% Stage I, 31% Stage II, 38% Stage III, and 2% Stage IV. The postoperative histologic examination indicated that chronic liver disease was present in 35% of the patients and microvascular tumor invasion was identified in 60% of the patients. The 90-day postoperative mortality rate was 4%. After a median follow-up time of 63 months, the 5-year overall survival rate was 40%. Patients treated with right hepatectomy (n = 332) and those requiring extended hepatectomy (n = 207) had similar 90-day postoperative mortality rates (4% and 4%, respectively, P = .976) and 5-year overall survival rates (42% and 36%, respectively, P = .523). Overall survival and postoperative mortality rates after major hepatectomy were similar among the participating countries (P > .1) and improved over time with 5-year survival rates of 30%, 40%, and 51% for the years 1981-1989, 1990-1999, and the most recent era of 2000-2008, respectively (P = .004) (Figure). Factors that were associated with worse survivals included AFP level > 1000 ng/mL, tumor size > 5 cm, presence of major vascular invasion, presence of extrahepatic metastases, positive surgical margins, and earlier time period in which the major hepatectomy was performed (all MV P < 0.05).
Conclusions: This multinational, long-term HCC survival analysis indicates that expansion of surgical indications to include major hepatectomy is justified by the significant improvement in outcomes over the past 3 decades observed in both the East and the West.
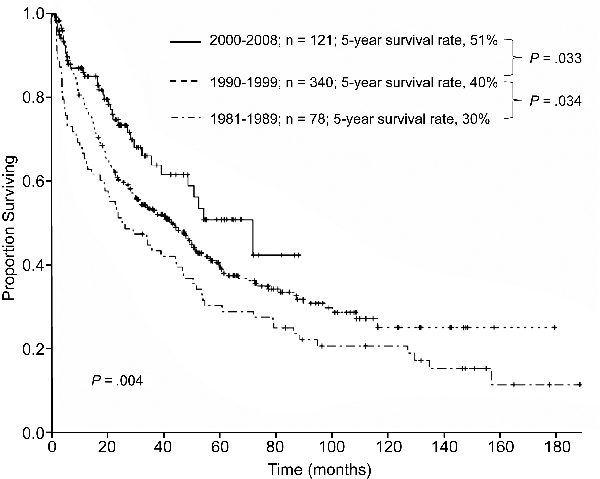
Improved Survivals After Major Resection of HCC Over Time
Back to Annual Meeting Program
|