|
Back to Annual Meeting Program
Visceral Fat Volume Better Than BMI At Risk Stratifying Colorectal Cancer Patients
Aaron S. Rickles*, James C. Iannuzzi, Andrew-Paul Deeb, Fergal Fleming, John R. Monson
Surgery, University of Rochester, Rochester, NY
Introduction:
The extent to which obesity effects colorectal cancer outcomes has been inconsistent in the literature, which may be a result of BMI being a poor descriptor of fat distribution. Compared to subcutaneous adipose tissue, visceral adipose tissue is more metabolically active, leading to a chronic inflammatory state and increasing the risk for diabetes, cardiovascular disease, and tumorigenesis. In addition, men and women distribute fat differently, thus leading to differences in outcomes based on BMI. The aim of this study is to describe the effect of visceral obesity on colorectal cancer outcomes between gender groups.
Methods:
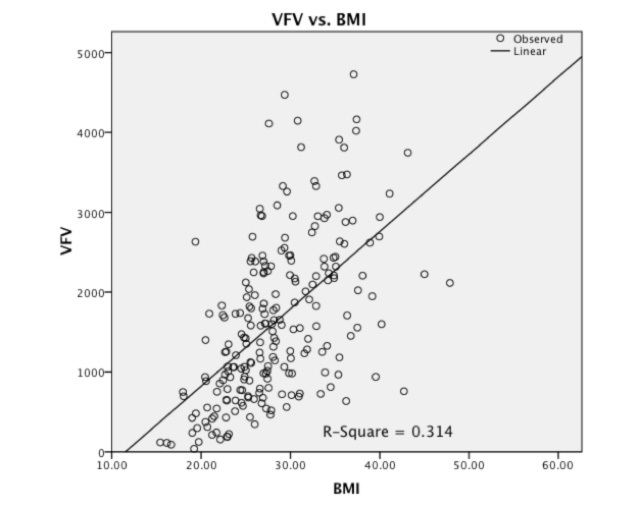
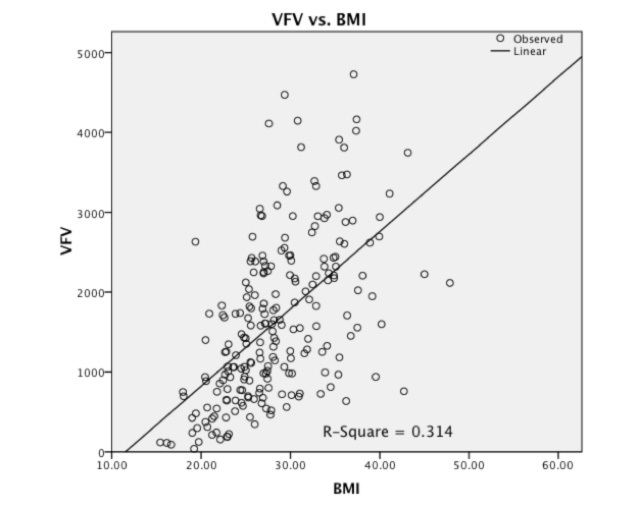
We conducted a retrospective chart review of colorectal cancer patients who underwent surgery at our institution between 2003 and 2010. Patient selection was restricted to those who had a pre-operative CT scan of the abdomen and pelvis. Exclusion criteria included emergency surgery, metastatic cancer, and patients with IBD or HNPCC. CT scans were used to measure visceral fat volume (VFV) using Carestream PACS 10.2 (Carestream Health, inc.). Patients with a BMI ≥ 30 were considered obese and viscerally obese patients were defined as those with a VFV greater than the mean. Linear regression was used to analyze the correlation between BMI and VFV, and independent sample t-test and Kaplan-Meier survival curves were used for outcome analysis.
Results:
A total of 233 patients met inclusion criteria, 75 Stage I (32%), 77 Stage II (33%), and 81 Stage III (35%). The mean age was 67, mean BMI 28.5, and mean VFV 1637cm3. There was no significant difference in BMI between males and females (28.1 vs. 28.9, p=0.294), however males had significantly more visceral fat than females (1867cm3 vs. 1371cm3, p=0.0001). In addition, BMI proved to be a poor descriptor of visceral obesity on linear regression (r2=0.314, see figure1). When analyzing disease free survival at three years (DFS3yr) there was no difference between obese and non-obese patients based on BMI. When analyzing outcomes based on VFV, non-obese females with Stage II cancer had significantly better DFS3yr compared to viscerally obese females (86.3% vs. 60.0%, p=0.034) although there was no significant difference in DFS3yr amongst males.
Conclusion:
This novel method for risk stratification demonstrates that visceral obesity decreases three year disease free survival for women with stage II colorectal cancer and should be considered in the discussion of chemotherapy use in these patients. Further study is necessary to delineate the effect of visceral obesity in men at various stages of colorectal cancer.
Figure 1: Linear regression of Visceral fat Volume and BMI.
Back to Annual Meeting Program
|