|
Back to Annual Meeting Program
Ostomy Creation Significantly Increases ER Visits and Hospital Readmission After Colorectal Resection
Lisa S. Poritz*1, Arthur Berg2
1Surgery, The Milton S. Hershey Medical Center, Hershey, PA; 2Biostatistics and Bioinformatics, The Milton S. Hershey Medical Center, Hershey, PA
Introduction: Readmission after colorectal (CR) surgery continues to be a significant problem and quality of care issue. The purpose of this study was to identify factors predictive of readmission after CR surgery.
Methods: 30% (computer generated list) of the records of all patients admitted to the CR service at our institution from July 2008-June 2011 were reviewed for patients undergoing colorectal resection. Patients who died within 60 days of surgery or were discharged to hospice were excluded. All others were then subdivided into 2 groups: those patients that were either re-admitted or visited the emergency room (ER) within 60 days after discharge and those patients that did not. Additional data abstracted from the medical record included total length of stay (LOS), post-operative LOS (POD), diagnosis subcategorized into malignant, diverticulitis, IBD, other benign disease; procedure subcategorized into colon resection, rectal resection, combined resection; presence of an ostomy, laparoscopic or open (converted procedures were in the open category), surgeon, admission type (urgent/emergent or elective), and patient age. Univariate and multivariate analysis was performed.
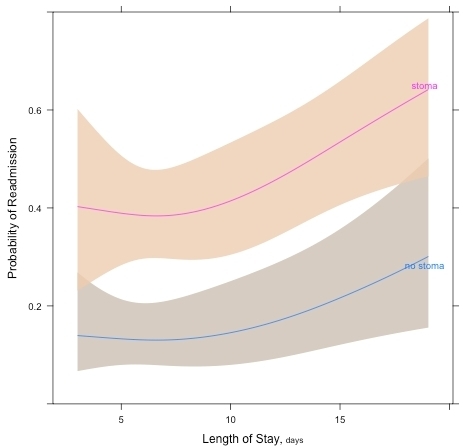
Results: 242 patients met criteria. Data is shown in the table. 74 (30.6%) patients were readmitted or visited the ER within 60 days of discharge. Diagnosis, type of resection, approach (lap vs open), age, and type of admission were not different between patients readmitted and those that were not. Presence of an ostomy (ileostomy or colostomy) was the most significant factor associated with readmission, with 77% of the readmitted patients having an ostomy (p=0.0000014). Surgeon performing the procedure, LOS, and POD, were also significant factors determining readmission on univariate analysis and all remained statistically significant on multivariate analysis. The most common reasons for readmission were nausea, vomiting, abdominal pain, and dehydration. 53/74 (72%) of the readmitted patients had at least one of these as their diagnosis. 129/242 (53%) of the patients in this series had an ostomy post-operatively, likely due to the large number of patients with IBD and rectal cancer. Emergent or urgent procedures were not a significant risk factor for ostomy creation. The image shows probability of readmission with increasing LOS for patients with and ostomy (top curve) and without (bottom curve). Bands are 95% confidence intervals.
Conclusions: The most significant predictive factor for readmission in this study was an ostomy. Ostomies are frequently used with elective and urgent CR and decreasing their use may not be prudent. However, the creation of each ostomy should be evaluated for necessity by the surgeon. Quality improvement projects should be directed at assessing readiness of ostomy patients for discharge and adequacy of support at home.
| Readmission | No Readmission | p value | | Total patients | 74 | 168 | | | Age (years, mean ± standard error) | 55.12 ± 1.94 | 55.71 ± 1.20 | 0.562 | | | | | | Diagnosis | | | 0.138 | | IBD | 27 | 45 | | | Malignancy | 30 | 77 | | | Diverticulitis | 8 | 33 | | | Other Benign | 9 | 13 | | | | | | | Type of resection | | | 0.255 | | Colon | 44 | 117 | | | Rectal | 27 | 44 | | | Multiple | 3 | 7 | | | | | | | Ostomy | | | | | Ileostomy/colostomy/no ostomy | 43/14/17 | 56/16/95 | 0.0000034 | | Any ostomy/no ostomy | 57/17 | 72/95 | 0.0000014 | | | | | | Open/Laparoscopic | 50/24 | 117/50 | 0.762 | | Surgeon | | | 0.0395 | | A | 22 | 75 | | | B | 14 | 28 | | | C | 9 | 26 | | | D | 29 | 38 | | | | | | | LOS (days, mean ± standard error) | 11.22 ± 1.22 | 7.49 ± 0.30 | 0.00608 | | POD (days, mean ± standard error) | 9.81 ± 1.09 | 6.79 ± 0.24 | 0.0168 | | Admission type | | | 0.363 | | Emergent/urgent | 16 | 28 | | | elective | 56 | 140 | |
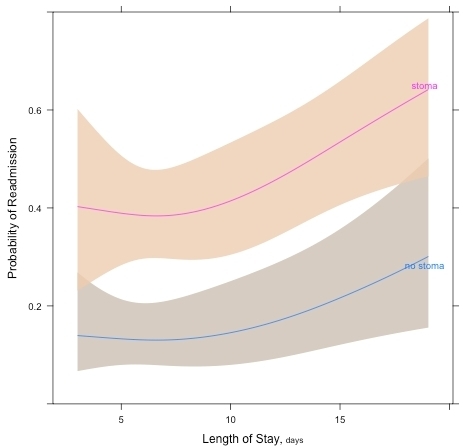
Probability of Readmission: Top line: with ostomy, bottom line: without ostomy Shaded areas are 95% confidence intervals
Back to Annual Meeting Program
|