Introduction: Anastomotic leak (AL) is one of the most feared complications following esophagectomy. Despite the complexity of the operation, the influence of the learning curve on AL has not been extensively studied. We sought to determine the predictors of esophageal AL with a particular focus on the learning curve. Methods: A prospective clinical database identified the first 100 esophagectomy patients by a single surgeon from 7/05-9/08. Patient and tumor characteristics, and operative variables were assessed for predictors of AL. Fisher’s or M-W U-test determined significance (*p<0.05). Multivariate logistic regression determined independent predictors. Cumulative Sum(CUSUM) analysis was use to generate a learning curve with unacceptable/acceptable leak rates set at 30%/10% and type I/II error at 0.05/0.20.Results: 92 cancers (ADC=66/SCC=16/Other=10) and 8 benign conditions were resected by Ivor-Lewis=37, 3-hole=19, laparoscopic=9, thoraco-abdo=23, and trans-abdo=12. AL was present in 14/100 and was more likely in the first 30 cases (8/30(26%) vs 6/70(8%))*, cervical anastomosis (8/28 vs 6/73)*, tube jejunostomy insertion (6/25 vs 7/74 - p=0.08), immediate post-op vasopressor use (4/16 vs 6/75 - p=0.07), and absence of anastomotic re-enforcement with pleura/omentum (14/82 vs 0/14 - p=0.09). Extent of resection (en-bloc 7/59 vs standard 7/41), anastomotic technique (hand-sewn 10/85 vs stapled 4/15), lymphadenectomy (D2 9/75 vs D1 5/25), or prior radiotherapy (3/10 vs 11/90), had no significant influence on AL. Independent predictors of AL included cervical anastomosis* and early surgeon experience (first 30 cases)*. The point of inflection of the CUSUM analysis curve was at the 34th case, after which the rate of anastomotic leak diminished significantly (see figure). Conclusions: Surgeon experience is a major predictor of AL following esophagectomy and represents an accumulation of a series of technical refinements and post-op management. By the 34th case of this complex procedure, an acceptable leak rate can be achieved by a dedicated esophageal program.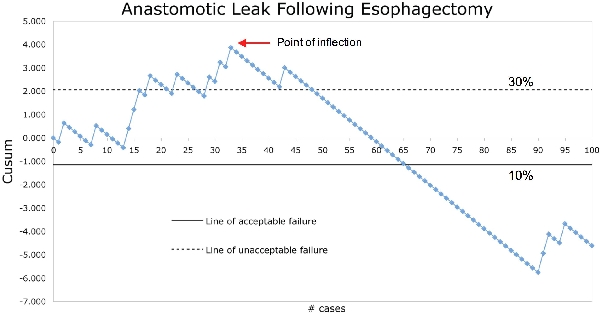
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461