Japan Pancreas Society has been conducting nation-wide pancreatic cancer registry since 1981. The definition of early pancreatic cancer is still controversial and current classification of pancreatic cancer divides in situ or intra-ductal carcinoma from invasive cancer though there must be contiguous process of invasion. Only 1.8% of invasive cancer is JPS-Stage I, while most of the patients have JPS-Stage IVa and IVb disease. Out of 908 patients with invasive pancreatic cancer less than 2 cm in size, only 177 (19.4%) patients had JPS-Stage I disease with median survival of 69.5 months. The survival of the patients with jaundice or back pain was significantly worth than that of patients who was diagnosed without symptom. Pancreatic cancer seems to gain its aggressiveness during growth evidenced by the increased ratio of poorly differentiated carcinoma, lymphatic infiltration, vascular infiltration and perineural infiltration. Even in small (<2 cm) tumor, the ratio of scirrhous carcinoma exceeded more than 30%, which was similar with larger tumors. The combined resection of peripancreatic plexus significantly increased the survival of patients with small (<2 cm) pancreatic cancer in the head of the pancreas. This effect was abrogated when the tumor exceeds 2cm in diameter. The 5-year survival rate of 288 patients after pancreatectomy for in situ intraductal papillary mucinous neoplasm (IPMN) was 81.9%. When the tumor invades microscopically the 5-year survival of 113 patients was decreased to 70.9%, while that of patients with invasive carcinoma derived from IPNM was 32.1%. The early diagnosis and treatment of pancreatic cancer is still challenging and the definition of early pancreatic cancer needs to be clarified.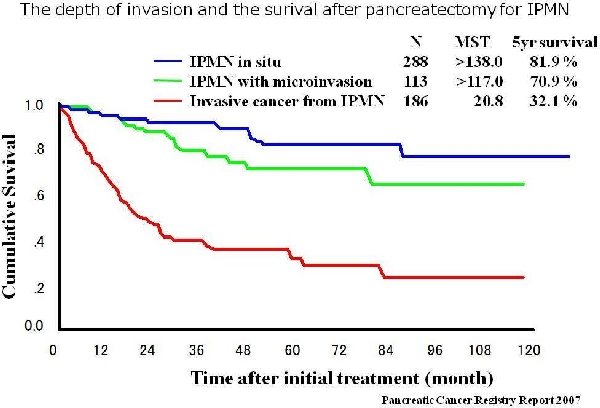
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461