PURPOSE: The hybrid laparoscopic-open procedure was devised as a means of providing benefits of minimally invasive methods to rectal cancer patients in whom a fully laparoscopic operation may not be feasible. Hybrid methods use a small infra-umbilical incision to perform open TME and cancer resection after closed splenic flexure mobilization, proximal devascularization, and division of the proximal bowel. Currently, we perform laparoscopic, hand-assisted and hybrid procedures. The purpose of this study is to assess the pathologic and long-term oncologic results of hybrid resection for rectal carcinoma.METHODS: We retrospectively reviewed pathologic and oncologic data from 75 patients who underwent hybrid rectal cancer resection at Columbia University from 1995 to 2004. Mean follow up was 3.3yrs. Half of our population had follow up for mean of 5.3yrs.RESULTS: Procedures included rectosigmoidectomy=10, LAR=49 and APR=15. Tumors were located in the proximal=28, middle=29 and distal=18 rectum. Anastomoses included EEA=57 and hand-sewn coloanal=3. Diverting stomas were used in 19 patients. Mean results of clinical and pathologic outcome data are: incision length 10cm (SD 4.5); days to flatus 3.8 (SD 2), length of stay 7.4days (SD 4), distal margin 3.2cm (SD 1.5), proximal margin 19.7cm (SD 7.2), lymph node harvest 14 (SD 7.5).5-year disease-free survival for hybrid rectal resections was 80%; 28 patients (37%) had preop XRT (figure).CONCLUSIONS: Hybrid rectal resections do not compromise LN harvest or margins and are feasible even in the context of neoadjuvant radiation therapy. Our 5-year disease-free survival of 80% is comparable to rates achieved by open surgery (64%, SEER data).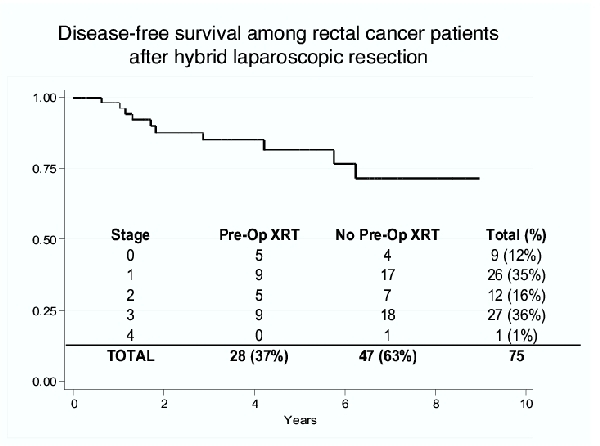
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461