Background: Pancreatoduodenectomy (PD) provides only chance for cure in patients with pancreas head cancer (PHC). However, owing to tumor aggressive nature and its anatomical proximity we often encounter portal venous involvement at the time of diagnosis. It is still not clear how far we can go with surgery, i.e. the clinical impact of simultaneous portal venous resection (PVR) for PHC remains controversial.Methods: We reviewed our pancreas database of 108 patients with PHC who underwent PD during 2001-2007. Of 108 patients 62 (57%) underwent PVR. We compared the short and long-term outcome between patients with PVR (Group A) and those without PVR (Group B). Results: Age, gender and type of procedure (standard or pylorus-preserving PD) were not different between the groups. Tumor factor (T) was more advanced in Group A by JPS classification but not different by UICC classification because of definition. Nodal involvement was not different between the groups (75% vs. 63%). Of 62 patients with PVR 42 (68%) patients had pathologically-proven portal vein involvement. Mortality (30-day and all hospital death) was 2.7% and 6.5% respectively, and notably all mortality were seen in Group A. Morbidity were commonly seen in Group A but not statistically different (47% vs. 39%). Postoperative adjuvant chemotherapy was used in 82% and 83%, respectively. R0 resection was achieved in 65% in Group A and 74% in Group B (NS). Median survival time (MST) was 15.8 months in Group A and 21.5 months in Group B (P=.06). If mortality cases were excluded MST was 18.0 months in Group A (Figure).Conclusion: Simultaneous PVR during PD for patients with PHC provides similar clinical benefit as compared with those patients without having a PVR if surgical mortality is minimal. Further refinement of surgical technique is necessary but further improvement of survival cannot be achieved without more effective adjuvant therapy.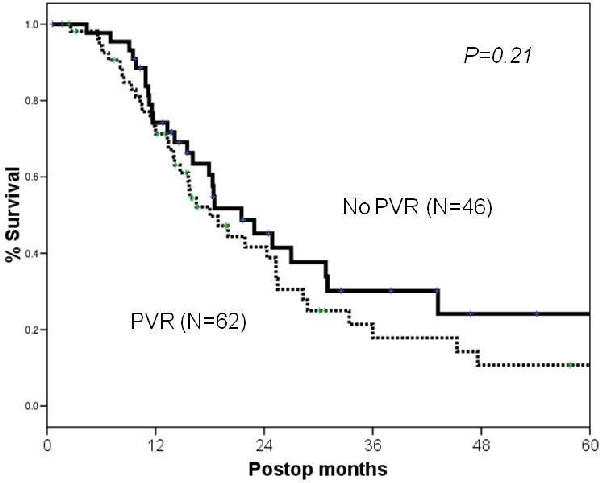
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461