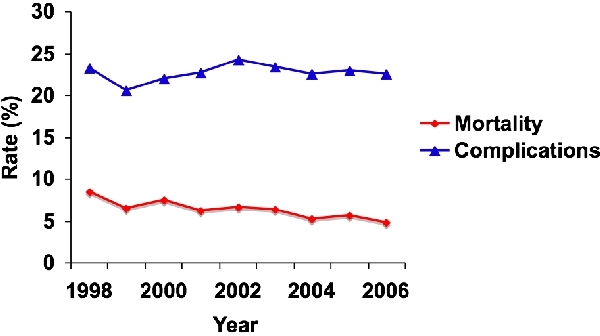
Introduction: National studies on in-hospital pancreatic outcomes have focused on mortality. Non-fatal morbidity might affect a substantially greater proportion of patients. Methods: The Nationwide Inpatient Sample 1998-2006 was queried for discharges after pancreatectomy. Rates of major complications, defined as myocardial infarction, aspiration pneumonia, pulmonary compromise, procedure-related perforation or laceration, infection (other than wound/pneumonia), DVT/PE, gastrointestinal hemorrhage, or reopening of laparotomy, were assessed. Age, sex, Charlson score, hospital procedure volume, indication for operation, and procedure type were evaluated for association with complication(s) using logistic regression. The independent effect of complications on in-hospital mortality, prolonged length of stay, and discharge disposition was also assessed.Results: Of 102,417 patient-discharges, 22.7% experienced a complication. Complication rates did not decline significantly over time, while mortality rates did (p<0.0001). On crude analysis, hospital resection volume was inversely correlated with complication rate and in-hospital death (p<0.0001). On multivariable analysis, predictors of complications included age ≥75 (referent, 19-39; adjusted odds ratio [OR] 1.3, 95% confidence interval [CI] 1.2-1.5, p<0.0001), Charlson of 4-7 (vs 0-1; OR 1.3, 95%CI 1.1-1.6, p=0.0006), total pancreatectomy (vs proximal, OR 1.3, 95%CI 1.1-1.5, p=0.0025), and low hospital volume (vs high, OR 1.6, 95%CI 1.4-1.8, p<0.0001) or medium (OR 1.4, 95%CI 1.2-1.5, p<0.0001). Complications were also a significant independent predictor of death (OR 7.8, 95%CI 6.7-8.8, p<0.0001), LOS (OR 6.9, 95%CI 6.2-7.7, p<0.0001), and discharge to another facility (OR 0.28, 95%CI 0.26-0.31, p<0.0001). Conclusions: Despite improvements in in-hospital mortality, major complication rates remain largely unchanged and represent a significant burden. Complications strongly predict in-hospital mortality, LOS, and delayed return to home. The impact on health care costs, quality of life, and long-term survival deserves further study.
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461