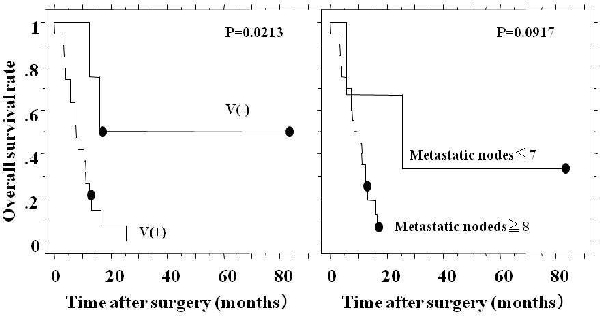
The lower thoracic (Lt) esophageal squamous cell carcinoma (ESCC) mainly metastasizes to abdominal lymph nodes. Although abdominal paraaortic lymph node (PAN) metastasis is often seen in patients with Lt ESCC, clinicopathological significance of PAN metastasis remains unknown. The purpose of this study was as follows; (1) to retrospectively analyze the frequency and extent of the lymph node metastasis in patients with Lt ESCC and (2) to clarify the clinicopathological characteristics of PAN (+) patients. A total of 283 patients with Lt ESCC underwent esophagectomy with lymphadenectomy at our hospital between April 1984 and March 2007. Of these 283 patients, 70 patients who underwent abdominal paraaortic lymph node dissection (PAND) (N=55) or PAN sampling (N=15) were retrospectively analyzed. Twenty-four patients had pathological PAN metastasis and the remaining 46 did not. Clinicopatholigical characteristics were compared between patients with PAN (+) and those with PAN (-). As compared with PAN (-) patients, PAN (+) patients had significantly more total number of metastatic nodes (25.2±26.4 vs 2.9±3.2, p<0.0001) and more venous invasion (20/24 vs 26/46, p=0.036). Overall survival of the PAN (+) patients was significantly poorer than PAN (-) patients (34.8% vs 73.1% at 1 year, 7.6% vs 52.7% at 3 years, p<0.0001). As regard with the recurrence patterns, PAN(+) patients had a significantly higher lymphatic (p<0.0001) and hematogeneous (p=0.0278) recurrences. Among the 24 PAN(+) patients, prognostic factor(s) was analyzed from several clinicopathological parameters. Venous invasion (v- vs v+) and the number of metastatic nodes (≦7 vs ≧8) were found to be prognostic factors. In conclusions, Lt ESCC with PAN (+) are considered to be a systemic disease and thus long term survival cannot be expected by surgical treatment.
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461