Introduction: Positive volume-outcomes relationships in esophagectomy have prompted support for regionalization of care; however broad US outcomes have not recently been analyzed. This study was designed to examine national trends in provision of esophagectomy and to reassess the volume-outcome relationship in light of changing practice patterns and training paradigms. Methods: Data were obtained from the Nationwide Inpatient Sample, the largest all-payer discharge database in the US, from 1998-2006. A search for total esophagectomy, partial esophagectomy and esophagogastrectomy was performed. Quantification of patients’ comorbidities was made using the Charlson Index. Using logistic regression modeling, annual case volumes were correlated with institutions’ outcomes. Arbitrarily-assigned case volume categories were avoided. Risk-adjusted outcome measures were calculated for mortality and various complications.Results: A total of 57,676 esophagectomies were recorded. Though patient demographics remained similar across the study period, in-hospital unadjusted mortality fell from 12% to 7%. Regionalization increased; hospitals performing > 20 esophagectomies per year increased from 22% to 28%, and hospitals with a case volume <12 decreased from 57% to 52%. Adjusting for comorbidities, greater case volume was associated with significant improvements of in-hospital mortality (p<.0001), post-operative shock (p=.0018), splenic injury (p=.0026), respiratory failure (p=.0027), pneumonia (p=.0035) and renal failure (p<.0001). Increasing benefit was seen with increasing volumes.Conclusions: The current mortality rate of 7% following esophagectomy is higher than that reported in most contemporary case series. Using national population-based data, the hypothesized positive volume-outcome relationship of esophageal surgery has been validated without the use of arbitrarily-assigned case volume categories. This relationship exists for all volumes of esophagectomy. The current paradigm of assuming improved outcomes as a result of the above parameters is justified.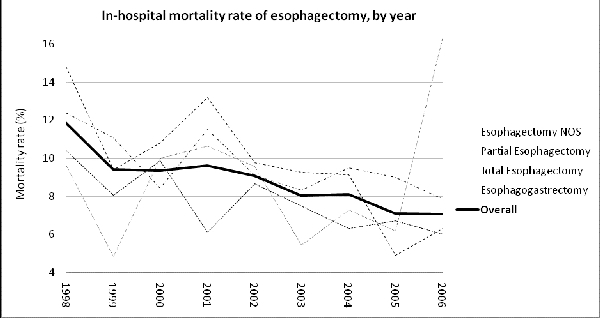
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461