Background: Direct objective measurements of the restrictive effect of various antireflux procedures are critical for achieving successful clinical outcomes. With the recent introduction of a method for intraoperative determination of distensibility of the gastroesophageal junction (GEJ) (Blom et al. J Gastointest Surg 2005;9:1318-1325) these measurements are now possible.
Aim: To compare the effect of the Dor procedure (DP) to that of Nissen fundoplication (NF) on pressure-volume curves as a measure of distensibility of the GEJ intraoperatively.
Methods: Intraluminal GEJ pressures commensurate to increasing levels of luminal distention using a previously described method (Shaker et al. Am J Physiol Gastrointest Liver Physiol 2004;287:G815-G821) were determined intraoperatively and used to construct the pressure-volume curves in 14 patients following NF(for reflux disease) and 7 patients after a DP (post myotomy for treatment of achalasia). An infinitely compliant bag mounted on a manometric catheter was placed in the GEJ and precipitously distended by infusion of 5-30 ml of room air by 5 ml increments. Intra-bag pressures were recorded and used for calculation of a distensibility coefficient (dV/dP).
Results: At each level of bag distention, corresponding GEJ intraluminal pressure was significantly higher following NF compared to DP (*p<0.05). Overall, the distensibility of the GEJ following DP was significantly higher compared to NF (p<0.05).
Conclusion: The DP is significantly less restrictive as evidenced by its higher distensibility compared to the NF. Intraoperative distensibility studies are feasible and can be helpful for objective assessment of the effect of antireflux procedures on GEJ function. Supported in part by NIH grants T32 DK61923 and R01 DK25731.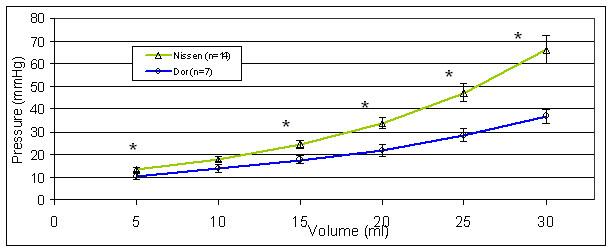
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461