Obesity, diabetes and hyperlipidemia are known risk factors for gallstone disease. However, the role that each of these factors play in this process remains unclear because most patients have two or all three of these problems. Recent studies from our laboratory in obese, diabetic mice have correlated body weight, serum glucose, insulin, cholesterol and triglycerides with poor gallbladder motility. In addition, a study in non-obese diabetic mice has demonstrated poor gallbladder emptying in young insulin resistant animals without frank diabetes. Moreover, a growing body of animal and human data have correlated insulin resistance with organ dysfunction. Therefore, we tested the hypothesis that non-obese, non-diabetic humans with insulin resistance would have gallbladder dysmotility.
METHODS:
Ninety-six lean, non-diabetic adult volunteers were studied. Blood was drawn, and gallbladder (GB) ultrasounds were performed before and after a standardized fatty meal. A GB ejection fraction (EF) was calculated, and an EF of <25% was considered abnormal. Serum was analyzed for cholesterol, triglycerides, cholecystokinin, leptin, glucose and insulin. The Homeostasis Assessment Model (HOMA) was used to determine insulin resistance. HOMA index = fasting glucose x fasting insulin/22.5 with insulin resistance defined as a HOMA index > 2.5.
RESULTS:
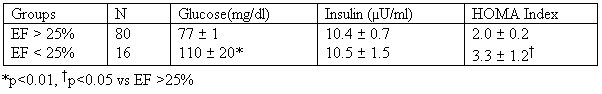
The volunteers had a mean age of 37 years (range 18-77), and 52% were female. The mean Body Mass Index (BMI) was 25 kg/m2 (range 19-29), and 37% had an elevated serum cholesterol. None of the volunteers had gallstones or biliary sludge, but 16 subjects (17%) had an EF <25%. Age, gender, weight, BMI, serum lipids, cholecystokinin, and leptin did not correlate with gallbladder dysmotility. Data for serum glucose, insulin and HOMA Index are shown in the table.
CONCLUSIONS:
These data suggest that lean, non-diabetic volunteers without gallstones have 1) a 17% incidence of impaired gallbladder emptying, and 2) gallbladder dysmotility is associated with an elevated fasting glucose as well as a high index of insulin resistance. We conclude that insulin resistance alone may be responsible for gallbladder dysmotility which may result in acalculous cholecystitis or gallstone formation.
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461