BACKGROUND: Gastric Bypass (GBP) results in durable weight loss and control of obesity-related co-morbidities. However, data attesting to survival benefits are few, and many primary care providers and insurers deny patients access on the rationale that GBP is a non-essential procedure. To better define the impact of GBP, we compared overall survival between morbidly obese patients who had operation at University of North Carolina Hospitals (UNC) and a control group of obese patients seen in the same institution for non-bariatric surgery care.
METHODS: Subjects included 313 patients who underwent GBP by a single surgeon (CAH) at UNC from 1982 to 1997. There were no body mass index (BMI) or payment restrictions applied, and all patients had active co-morbidities. Mean BMI was 50.2 +/- 11.3 kg/m2, and mean follow-up was 18.0 +/- 3.7 years. In creating a control group, UNC electronic databases spanning 1984-1997 were queried. To ensure surgery patients were as obese, we included in the control group all patients with either ICD code 278.00 for obesity (coded since 1984) or 278.01 for morbid obesity (coded since 1994). To ensure surgery patients were as likely to have co-morbidities, we included in the control group both outpatients and inpatients. Controls totaled 3,664, with mean follow-up 14.9 +/- 3.1 years. Occurrence of death was determined using the US Social Security Death Index, and survival was measured from the date of surgery for subjects, or from the first obesity diagnosis for controls, until date of death or 11/26/04. Groups were compared for variations in race and sex by the chi-square test, and for age differences by the t-test. Kaplan-Meier curves were generated and survival was compared by the log-rank test. To adjust for differences in age, race, and sex, proportional hazard regression was performed. RESULTS: The GBP group had greater survival than the control group (p<0.0001) (Figure). GBP patients were more likely to be female (p<0.0001), white (p<0.0001) and younger (p<0.0001). After adjusting for age, race, and sex differences, the GBP group still had superior survival, with a hazard ratio of 0.20 versus the control group (p<0.0001).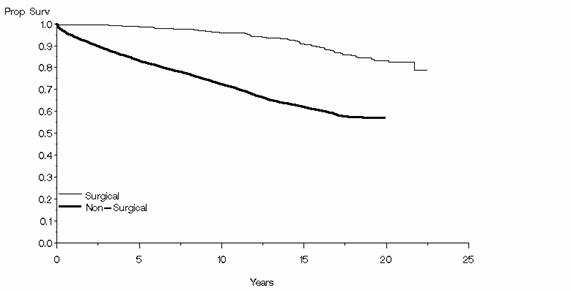 CONCLUSION: GBP for morbid obesity improves long-term survival, with patients demonstrating one-fifth the risk of death of a control group over twenty-year follow-up. Given recent federal recognition of morbid obesity as a disease, and survival data such as these, GBP must be considered a mainstream therapy.
CONCLUSION: GBP for morbid obesity improves long-term survival, with patients demonstrating one-fifth the risk of death of a control group over twenty-year follow-up. Given recent federal recognition of morbid obesity as a disease, and survival data such as these, GBP must be considered a mainstream therapy.
 500 Cummings Center
500 Cummings Center +1 978-927-8330
+1 978-927-8330
 +1 978-524-0461
+1 978-524-0461